Kidney disease is a very common health problem around the world. About 10% of the world’s population suffers from chronic kidney disease. In Sri Lanka approximately 1 in 5 people suffer from some form of kidney disease. approximately 90% of those with CKD don’t even know they have it. eventually those with kidney disease end up with end stage kidney failure,if not detected early. When kidneys lose their function they have difficulty eliminating waste products and fluid from the body. Patients with end stage failure can survive for longer periods of time and have a better quality of life with treatments such as dialysis and kidney transplants.
Western Hospital provides excellent care for patients (both adults and children) with kidney disease. As the pioneer is dialysis and kidney transplantation in sri lanka we take great pride in our highly experienced staff who perform dialysis and kidney transplants and help you achieve optimal kidney health.
Kidney Transplant
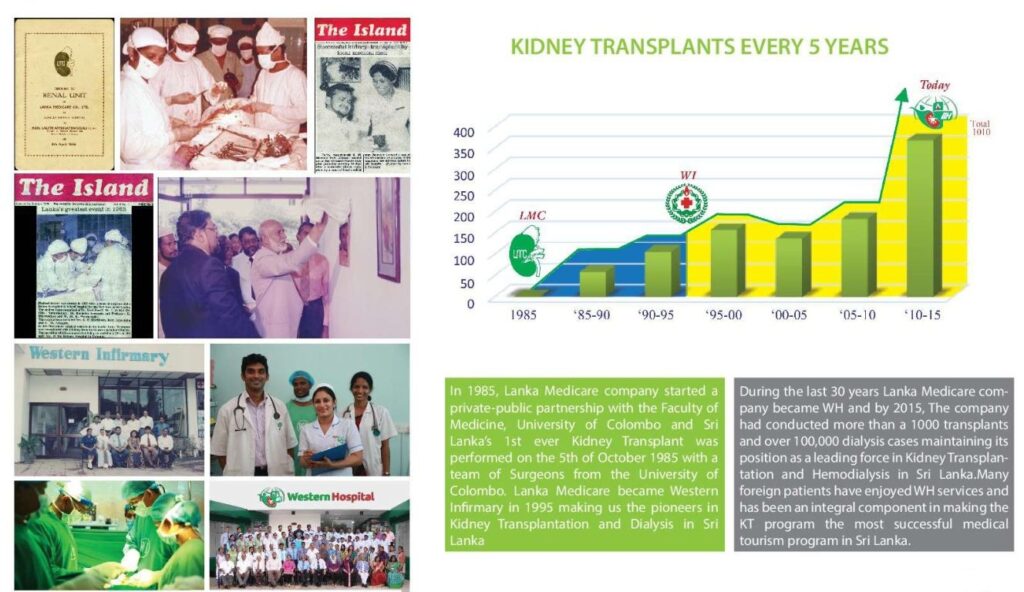
A kidney transplant improves the quality of life for patients that have end-stage kidney failure. Western Hospital has the longest running kidney transplant program in Sri Lanka; we performed the first kidney transplant in Sri Lanka in 1985, and have successfully completed over 1500 local & international kidney transplants since then. Given our experience, expertise and efficiency, opting for a kidney transplantation in Sri Lanka, Western Hospital is a reliable solution.